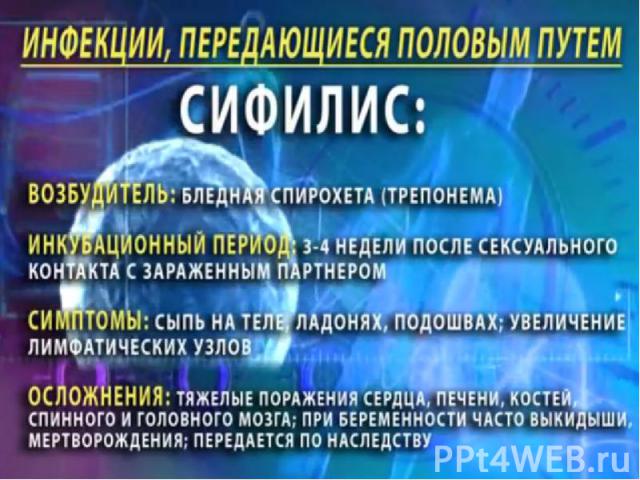
Презентация на тему: СИФИЛИС
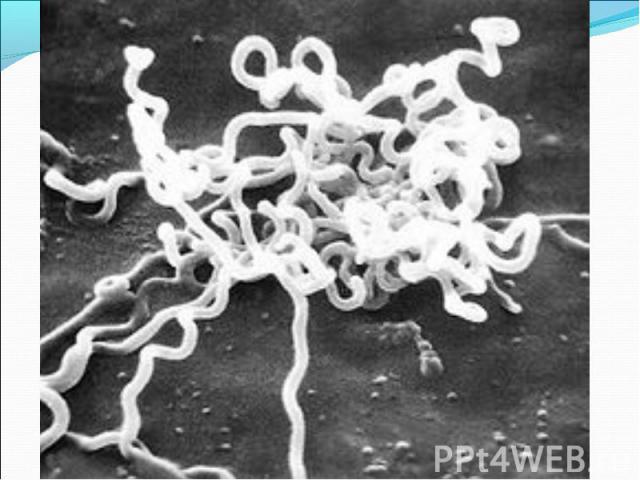
(возбудитель - бледные трепонемы) (возбудитель - бледные трепонемы)
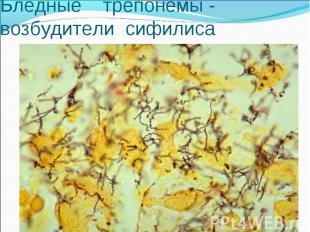
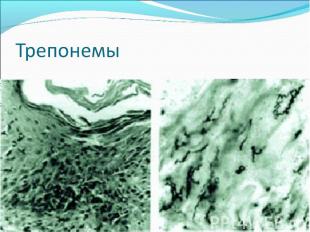
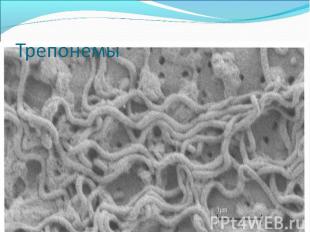

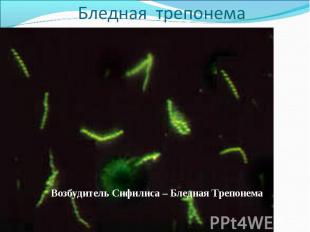
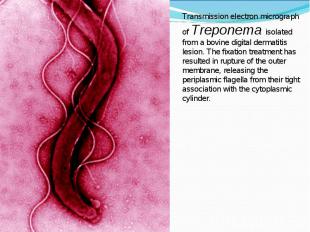





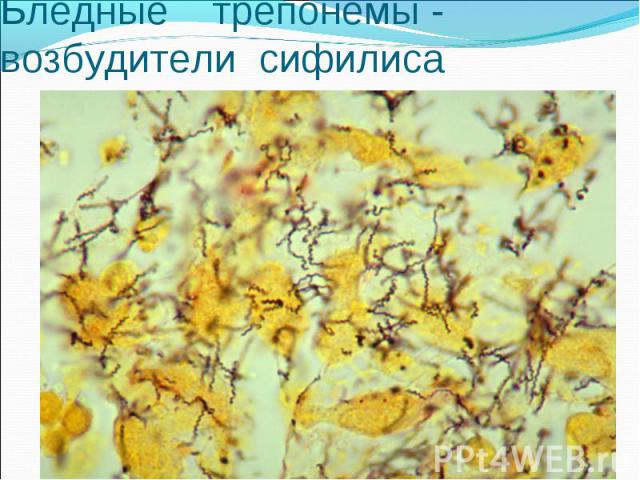
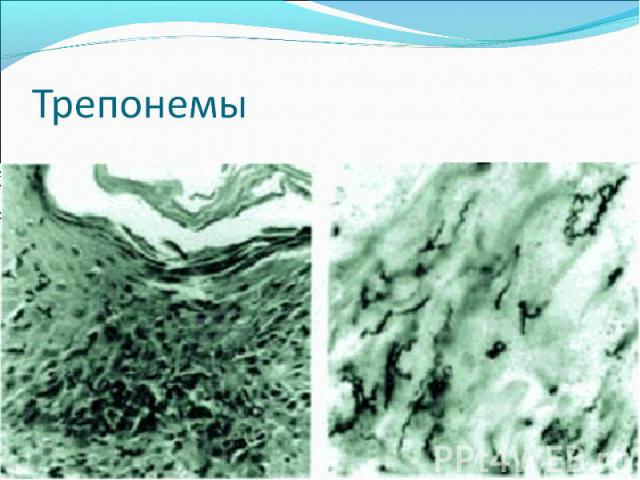
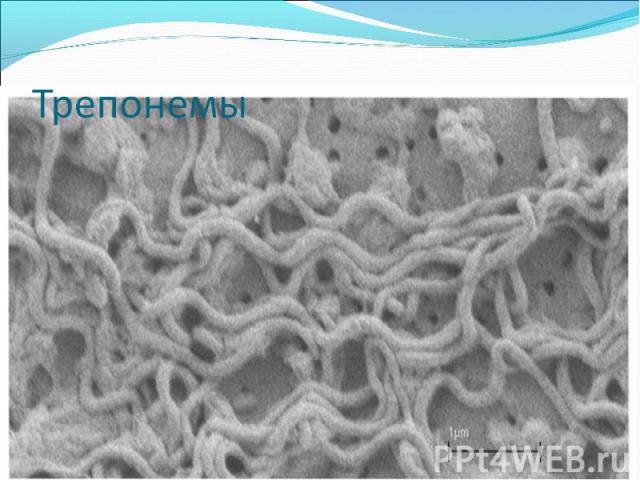
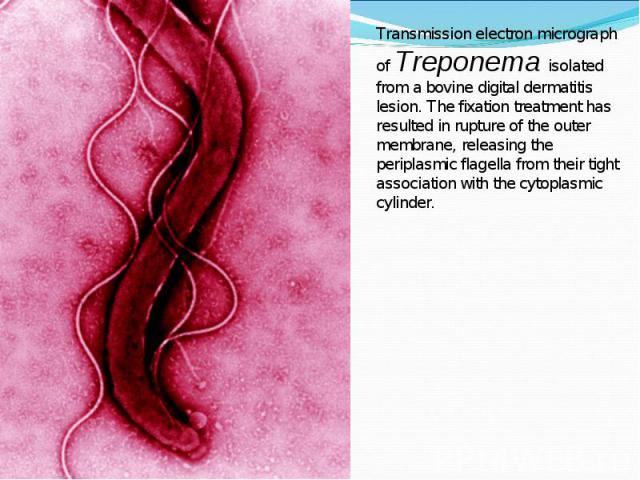
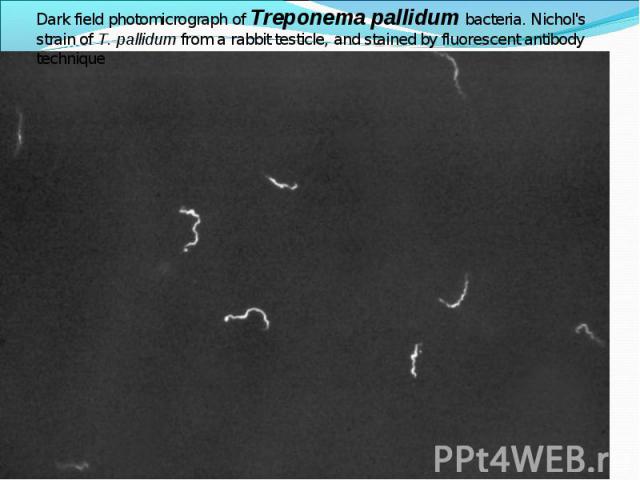
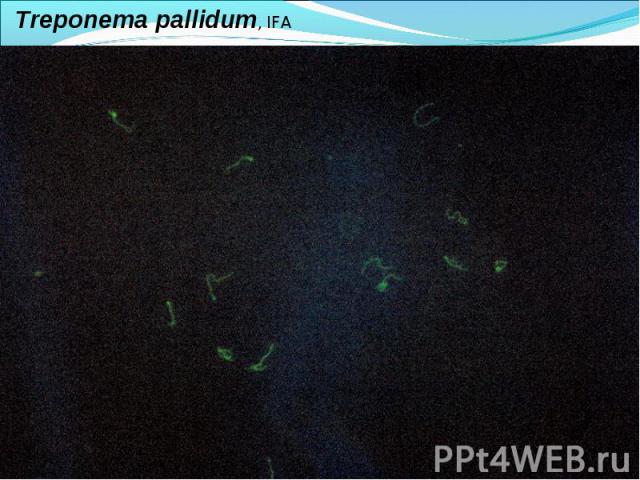
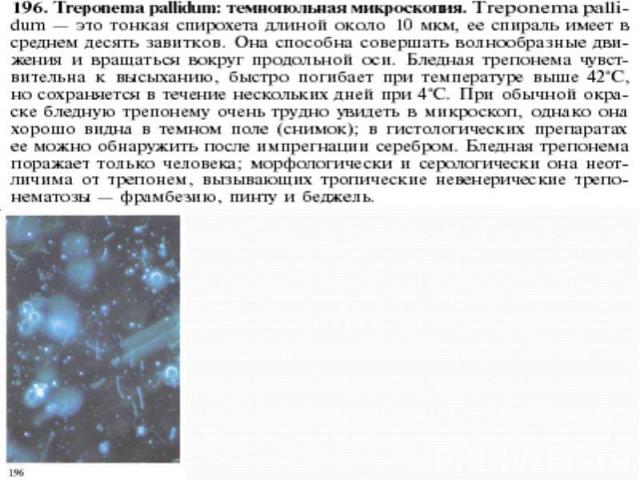
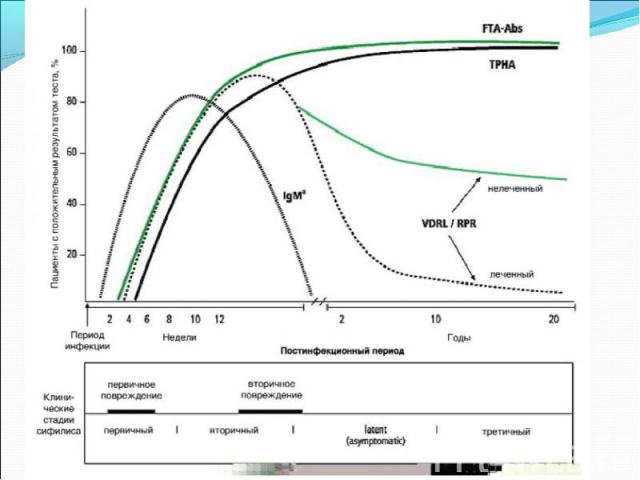
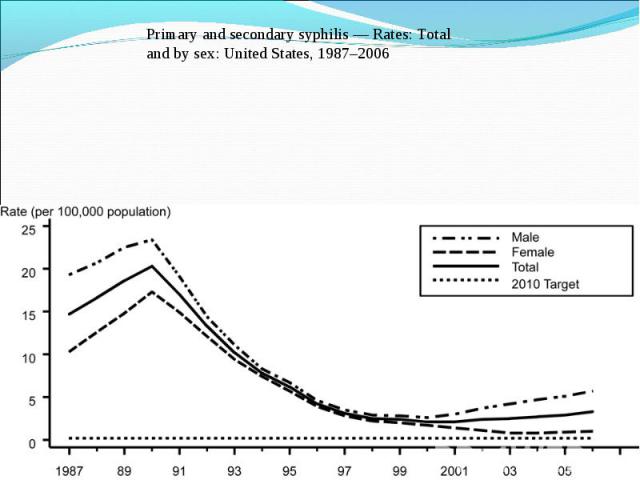
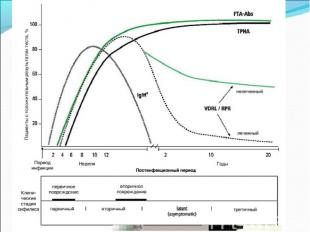
Diagnosis of syphilis The definitive diagnosis of primary syphilis is made by visualization of treponemes by dark field microscopy or by direct immunofluorescence (figure 18-19). The yield of these tests is high provided that (1) there is no prior topical or systemic antibiotic treatment and that (2) the examination is done by an experienced person. To obtain a specimen, the lesion can be gently abraded with gauze. The serous exudate is then applied to a glass slide. Direct or indirect immunofluorescence is recommended for oral lesions as non-pathogenic treponemes may be confused with T. pallidum on darkfield microscopy. Diagnosis of syphilis The definitive diagnosis of primary syphilis is made by visualization of treponemes by dark field microscopy or by direct immunofluorescence (figure 18-19). The yield of these tests is high provided that (1) there is no prior topical or systemic antibiotic treatment and that (2) the examination is done by an experienced person. To obtain a specimen, the lesion can be gently abraded with gauze. The serous exudate is then applied to a glass slide. Direct or indirect immunofluorescence is recommended for oral lesions as non-pathogenic treponemes may be confused with T. pallidum on darkfield microscopy. Serological tests are the most widely used tests for syphilis and are categorized into treponemal and non-treponemal tests. The non-treponemal tests detect anti-cardiolipin antibodies and include RPR (Rapid Plasma Reagin), Toluidine Red Unheated Serum Test (TRUST) and Reagin Screen test (RST), VDRL (Venereal Disease Research Laboratory) and Unheated Serum Reagin (USR). The sensitivity of the non-treponemal tests varies from 70% in primary syphilis to 100% in secondary syphilis. These tests are advantageous because they are inexpensive, applicable for screening purposes, and their titers tend to correlate with disease activity. However, confirmation of the non-treponemal tests is necessary with the specific treponemal tests. The FTA-ABS (fluorescent treponemal antibody absorption test), the MHA-TP (microhemagglutination assay) and the TP-PA (particle agglutination assay) are 80% to 100% sensitive depending on the stage of disease. However, a positive MHA-TP alone does not establish the diagnosis of primary syphilis in a patient with genital ulcer, since the MHA-TP can remain positive for life. Patients suspected of having primary syphilis with a negative darkfield examination, negative RPR and MHA-TP should have follow up serologies in 2 weeks, since detection by direct microscopy depends on specimen collection and the expertise of the microscopist, and since serologies can be negative in the first two weeks after a chancre appears. False-positive non-treponemal and treponemal tests can occur in a variety of disease conditions including acute viral infections, autoimmune diseases, vaccination, drug addiction and malignancy. Latent syphilis is diagnosed when a patient has a reactive RPR and a confirmatory test in the absence of signs or symptoms. The duration of disease from exposure can be estimated if the patient can recall specific signs or symptoms consistent with primary syphilis, has a history of exposure or previous serology. However, the usual scenario is that of a patient with positive serology and no clinical history suggestive of syphilis.






















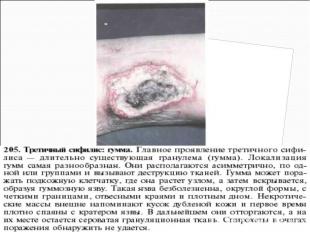



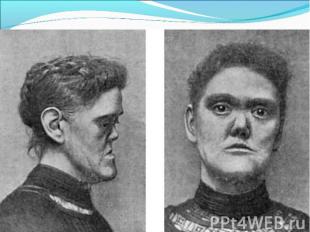
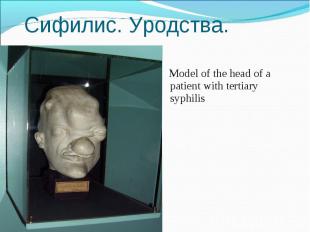
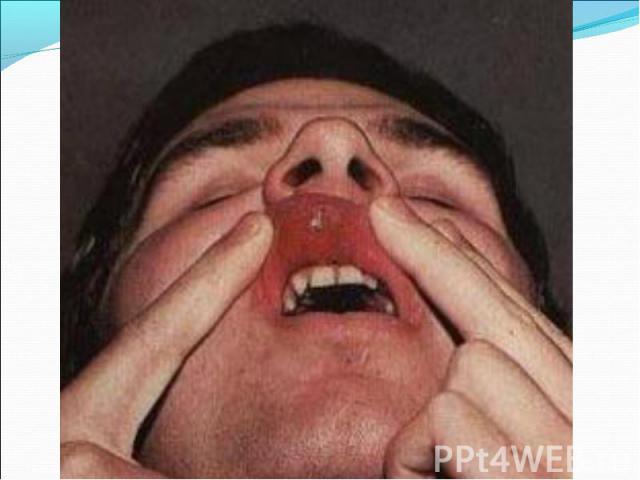
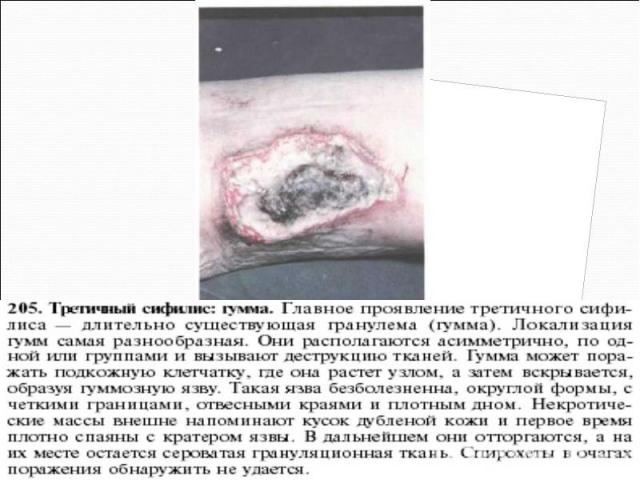
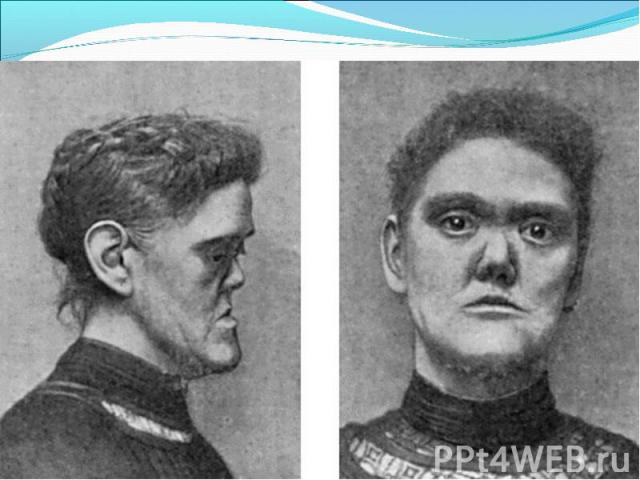
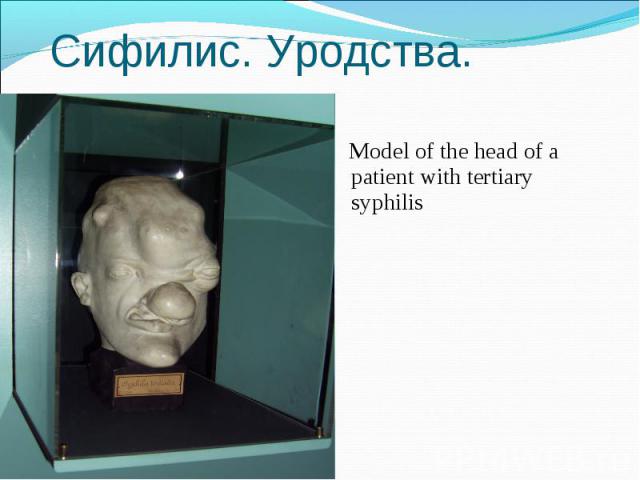
Model of the head of a patient with tertiary syphilis Model of the head of a patient with tertiary syphilis
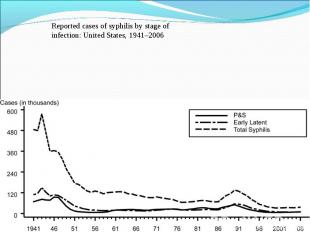
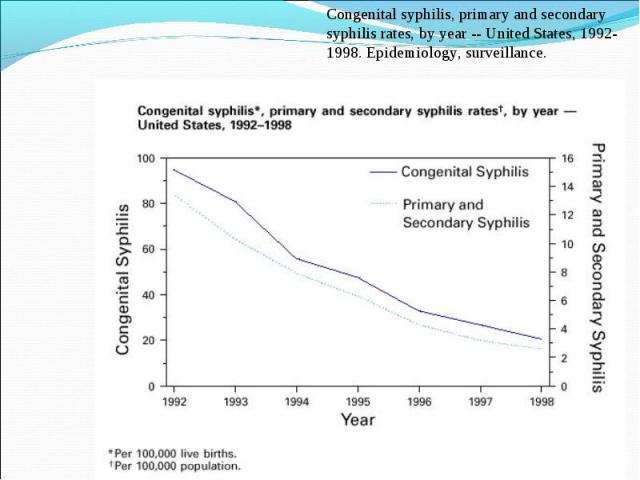
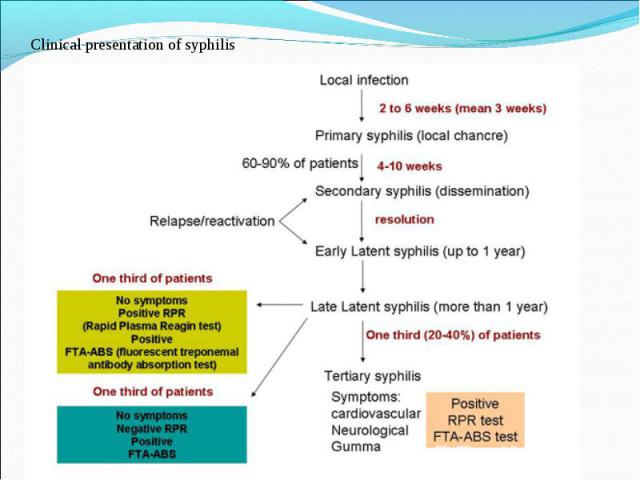
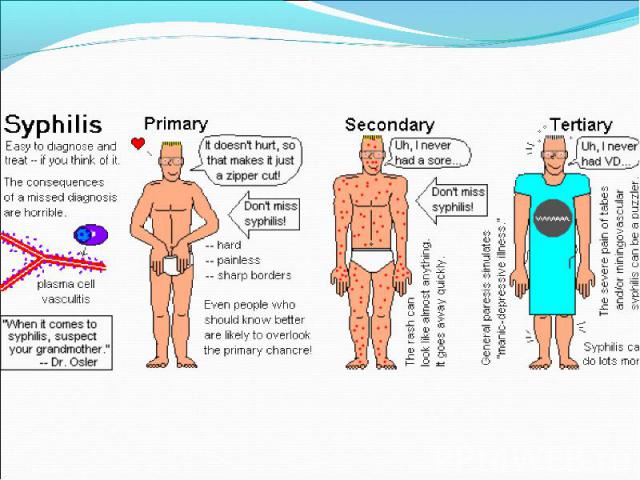
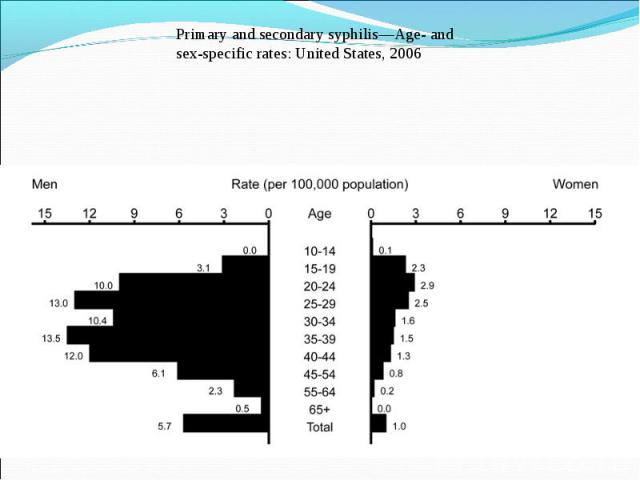
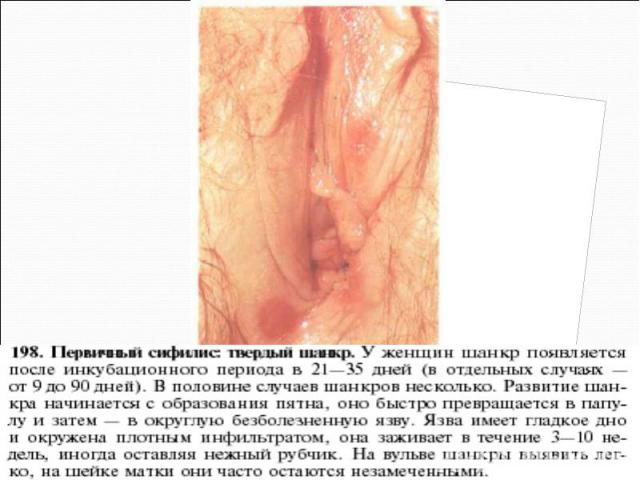
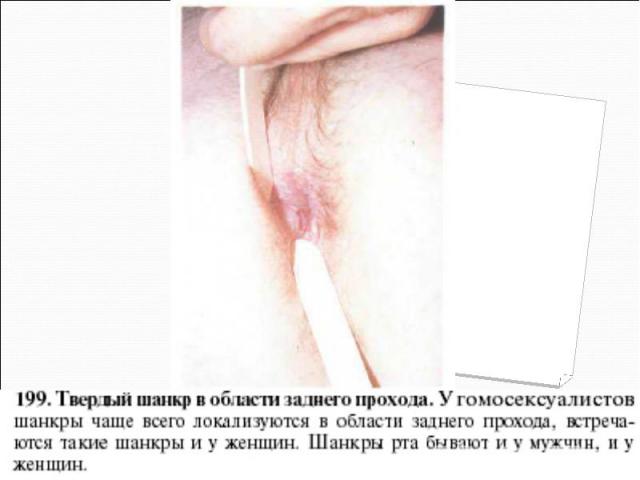
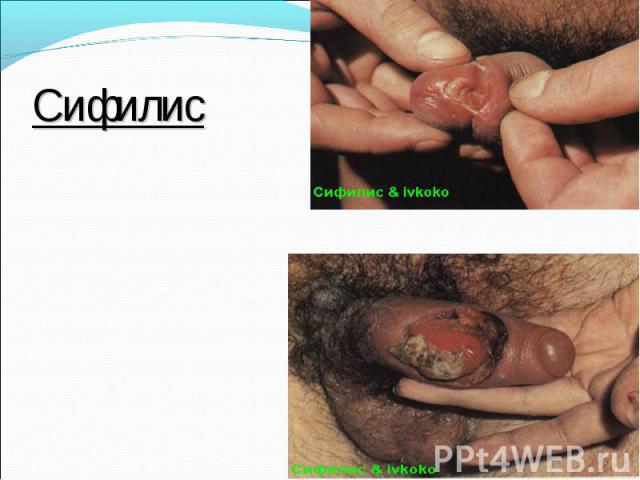
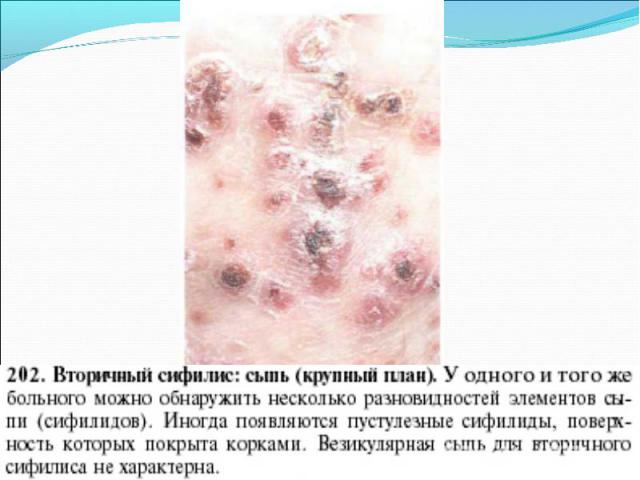
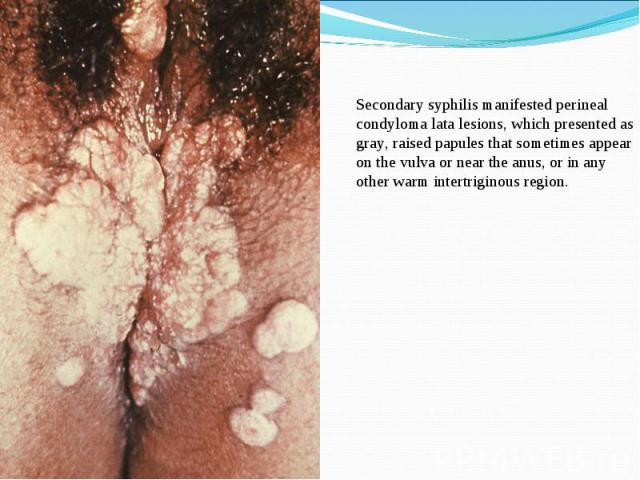
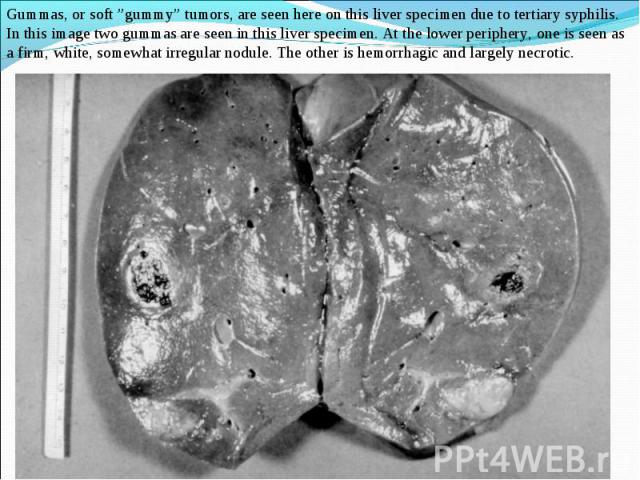
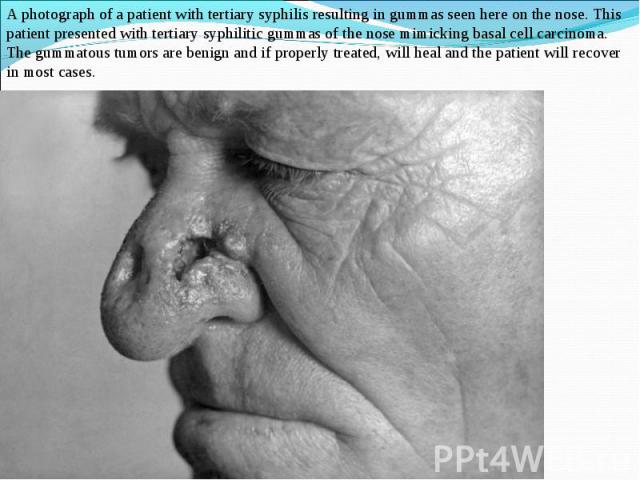
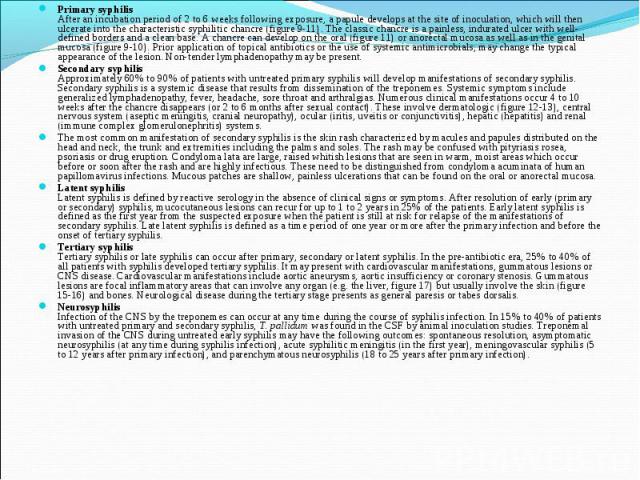
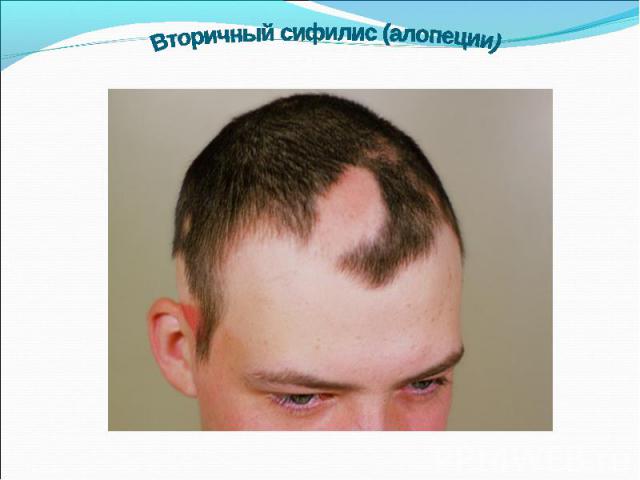
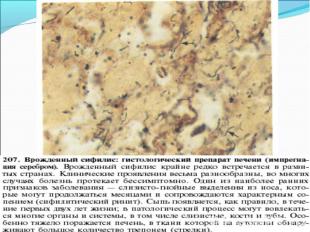
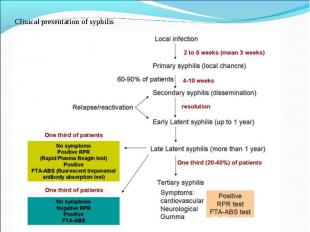
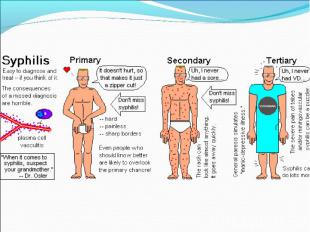
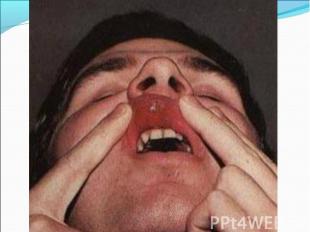
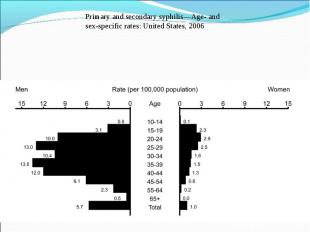
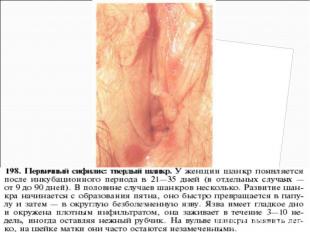
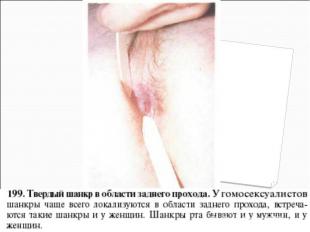
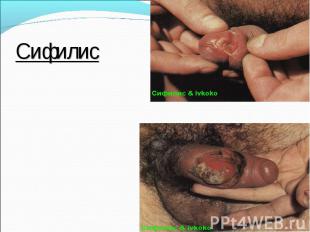
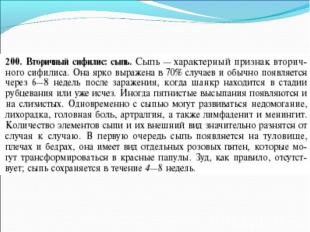
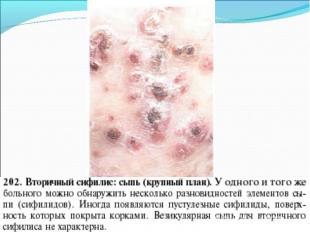
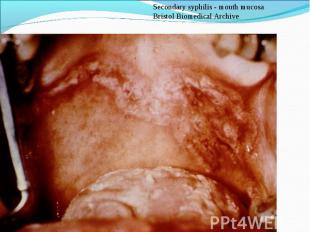
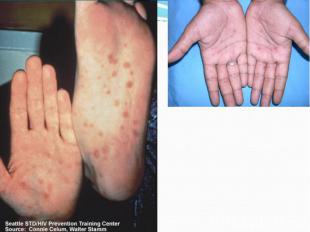
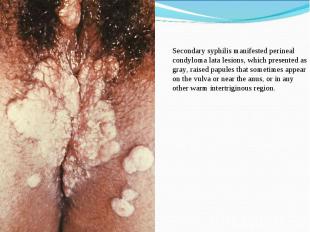
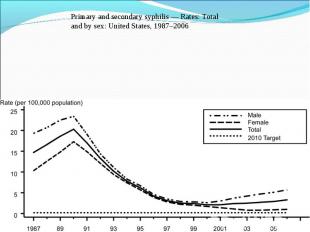
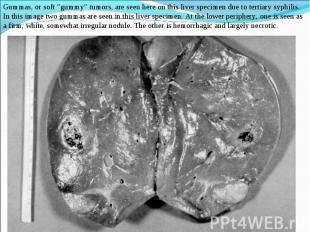
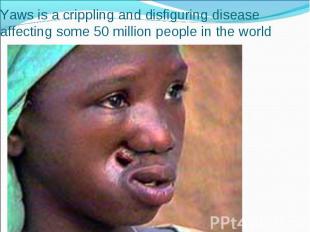
Primary syphilis After an incubation period of 2 to 6 weeks following exposure, a papule develops at the site of inoculation, which will then ulcerate into the characteristic syphilitic chancre (figure 9-11). The classic chancre is a painless, indurated ulcer with well-defined borders and a clean base. A chancre can develop on the oral (figure 11) or anorectal mucosa as well as in the genital mucosa (figure 9-10). Prior application of topical antibiotics or the use of systemic antimicrobials, may change the typical appearance of the lesion. Non-tender lymphadenopathy may be present. Primary syphilis After an incubation period of 2 to 6 weeks following exposure, a papule develops at the site of inoculation, which will then ulcerate into the characteristic syphilitic chancre (figure 9-11). The classic chancre is a painless, indurated ulcer with well-defined borders and a clean base. A chancre can develop on the oral (figure 11) or anorectal mucosa as well as in the genital mucosa (figure 9-10). Prior application of topical antibiotics or the use of systemic antimicrobials, may change the typical appearance of the lesion. Non-tender lymphadenopathy may be present. Secondary syphilis Approximately 60% to 90% of patients with untreated primary syphilis will develop manifestations of secondary syphilis. Secondary syphilis is a systemic disease that results from dissemination of the treponemes. Systemic symptoms include generalized lymphadenopathy, fever, headache, sore throat and arthralgias. Numerous clinical manifestations occur 4 to 10 weeks after the chancre disappears (or 2 to 6 months after sexual contact). These involve dermatologic (figure 12-13), central nervous system (aseptic meningitis, cranial neuropathy), ocular (iritis, uveitis or conjunctivitis), hepatic (hepatitis) and renal (immune complex glomerulonephritis) systems. The most common manifestation of secondary syphilis is the skin rash characterized by macules and papules distributed on the head and neck, the trunk and extremities including the palms and soles. The rash may be confused with pityriasis rosea, psoriasis or drug eruption. Condyloma lata are large, raised whitish lesions that are seen in warm, moist areas which occur before or soon after the rash and are highly infectious. These need to be distinguished from condyloma acuminata of human papillomavirus infections. Mucous patches are shallow, painless ulcerations that can be found on the oral or anorectal mucosa. Latent syphilis Latent syphilis is defined by reactive serology in the absence of clinical signs or symptoms. After resolution of early (primary or secondary) syphilis, mucocutaneous lesions can recur for up to 1 to 2 years in 25% of the patients. Early latent syphilis is defined as the first year from the suspected exposure when the patient is still at risk for relapse of the manifestations of secondary syphilis. Late latent syphilis is defined as a time period of one year or more after the primary infection and before the onset of tertiary syphilis. Tertiary syphilis Tertiary syphilis or late syphilis can occur after primary, secondary or latent syphilis. In the pre-antibiotic era, 25% to 40% of all patients with syphilis developed tertiary syphilis. It may present with cardiovascular manifestations, gummatous lesions or CNS disease. Cardiovascular manifestations include aortic aneurysms, aortic insufficiency or coronary stenosis. Gummatous lesions are focal inflammatory areas that can involve any organ (e.g. the liver, figure 17) but usually involve the skin (figure 15-16) and bones. Neurological disease during the tertiary stage presents as general paresis or tabes dorsalis. Neurosyphilis Infection of the CNS by the treponemes can occur at any time during the course of syphilis infection. In 15% to 40% of patients with untreated primary and secondary syphilis, T. pallidum was found in the CSF by animal inoculation studies. Treponemal invasion of the CNS during untreated early syphilis may have the following outcomes: spontaneous resolution, asymptomatic neurosyphilis (at any time during syphilis infection), acute syphilitic meningitis (in the first year), meningovascular syphilis (5 to 12 years after primary infection), and parenchymatous neurosyphilis (18 to 25 years after primary infection).