Презентация на тему: The Audit Process
The Audit Process
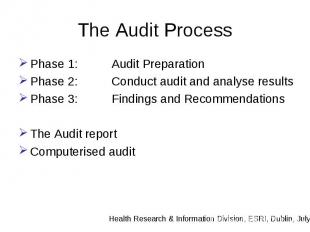
The Audit Process Phase 1: Audit Preparation Phase 2: Conduct audit and analyse results Phase 3: Findings and Recommendations The Audit report Computerised audit
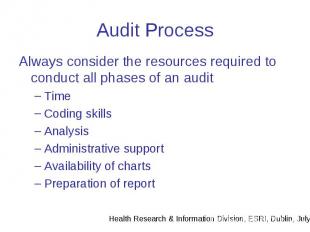
Audit Process Always consider the resources required to conduct all phases of an audit Time Coding skills Analysis Administrative support Availability of charts Preparation of report
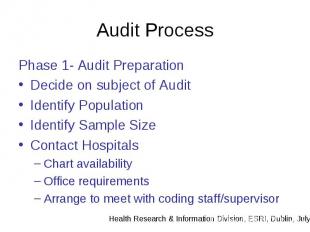
Audit Process Phase 1- Audit Preparation Decide on subject of Audit Identify Population Identify Sample Size Contact Hospitals Chart availability Office requirements Arrange to meet with coding staff/supervisor
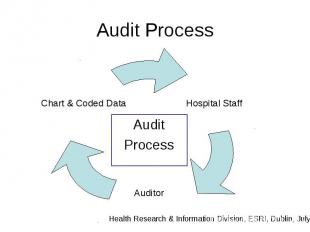
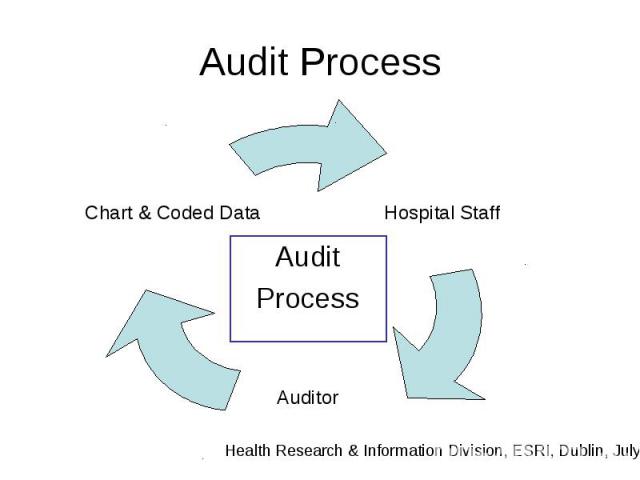
Audit Process Audit Process
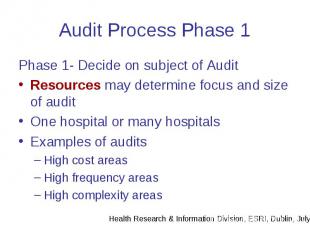
Audit Process Phase 1 Phase 1- Decide on subject of Audit Resources may determine focus and size of audit One hospital or many hospitals Examples of audits High cost areas High frequency areas High complexity areas
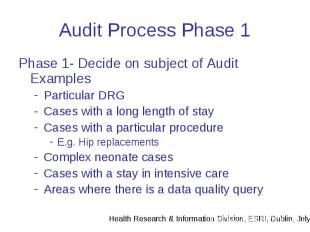
Audit Process Phase 1 Phase 1- Decide on subject of Audit Examples Particular DRG Cases with a long length of stay Cases with a particular procedure E.g. Hip replacements Complex neonate cases Cases with a stay in intensive care Areas where there is a data quality query
Audit Process Phase1 Phase 1: Identify population and sample size Population= The entire number of cases that meet the chosen criteria for the subject of the audit When the population is known the sample size can be determined
Audit Process Phase 1 Phase 1: Identify population and sample size Sample size: The number of cases to be audited Note: Resources may influence the sample size
Audit Process Phase 1 Phase 1: Identify population and sample size Sample Size: Must be practical 5% of one months discharges is a statistically acceptable sample size for a chart based audit (Source Australian Coding Benchmark Audit, 2nd Edition, NCCH, Sydney)
Audit Process Phase 1 Phase 1: Identify population and sample size Suggested Sample Size: General Audit = Minimum of 40 charts Targeted audits = Audits on specific topics can have a smaller sample size
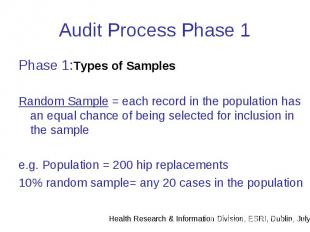
Audit Process Phase 1 Phase 1:Types of Samples Random Sample = each record in the population has an equal chance of being selected for inclusion in the sample e.g. Population = 200 hip replacements 10% random sample= any 20 cases in the population
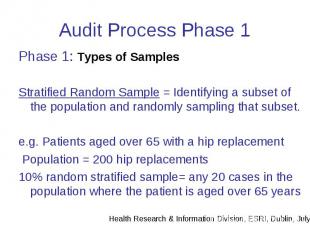
Audit Process Phase 1 Phase 1: Types of Samples Stratified Random Sample = Identifying a subset of the population and randomly sampling that subset. e.g. Patients aged over 65 with a hip replacement Population = 200 hip replacements 10% random stratified sample= any 20 cases in the population where the patient is aged over 65 years
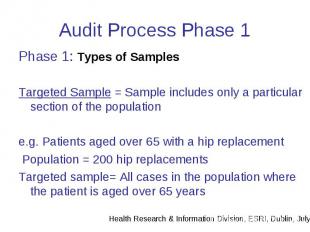
Audit Process Phase 1 Phase 1: Types of Samples Targeted Sample = Sample includes only a particular section of the population e.g. Patients aged over 65 with a hip replacement Population = 200 hip replacements Targeted sample= All cases in the population where the patient is aged over 65 years
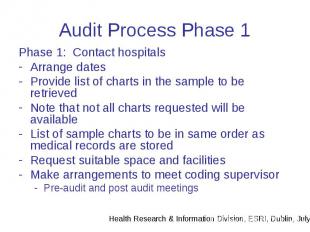
Audit Process Phase 1 Phase 1: Contact hospitals Arrange dates Provide list of charts in the sample to be retrieved Note that not all charts requested will be available List of sample charts to be in same order as medical records are stored Request suitable space and facilities Make arrangements to meet coding supervisor Pre-audit and post audit meetings
Audit Process Phase 2 Phase 2: Reabstraction Grouping Comparing codes
Audit Process Phase 2 Phase 2: Reabstraction Will original codes be visible to auditor? Will there be a audit data collection sheet? Will additional information be collected? e.g. Presence of discharge summary Documentation issues
Audit Process Phase 2 Phase 2: Reabstraction Adherence to guidelines Assessment of completeness of chart Meet with coding staff – Opportunity for discussion of code differences Preliminary findiongs and outline of next stage in process Identify local issues that may affect coding
Audit Process Phase 2 Phase 2: Grouping If DRG analysis is required then recoded cases must be grouped into DRGs Access to grouper and sytem for regrouping to allow for comparison at DRG and MDC level
Audit Process Phase 2 Phase 2: Comparing Codes Compare original codes to re abstracted codes Compare original administrative data to re-abstracted data Compare DRG assignment between original codes and re-abstracted codes.
Audit Process Phase 2 Phase 2: Comparing Codes Diagnoses: Identify Differences e.g. Differences in Principal Dx Differences in Additional Dx Compare Average number of Dx Differences in Sequencing of codes Diagnoses frequency Procedures
Audit Process Phase 2 Phase 2: Comparing Codes Identify differences in administrative data Date of birth Admission & Discharge dates Admission code Discharge code
Audit Process Phase 2 Phase 2: Comparing Codes Facility to record why codes are different. Helps to identify factors affecting coding quality e.g. Original coding PDx= Abdominal Pain Re abstracted PDx= Appendicitis Reason for difference: Original coder recorded symptom as Principal diagnosis and appendicitis as additional code
Audit Process Phase 2 Phase 2: Comparing Codes Factors affecting coding quality can include: Documentation Discharge summaries Information on ventilation Information on ICU stay Coder training levels Knowledge of coding guidelines Correct use of Classification Support for coding function How will these factors be recorded?
Audit Process Phase 2 Phase 2: Comparing Codes Identify how many differences in each data field And the reason for the difference
Audit Process Phase 2 Phase 2: Compare DRG assignment Identify differences in DRG assignment DRG frequency Change in severity of DRG Identify differences in MDC assignment
Audit Process Phase 3 Phase 3: Findings & Recommendations Having compared data make findings and recommendations based on evidence found by the audit process E.g. 70% of cases record a different Principal diagnoses due to poor documentation.
Audit Process Phase 3 Phase 3: Findings & Recommendations Highlight any areas with major differences Highlight system problems found to affect data quality Draw conclusions based on findings
Audit Process Phase 3 Phase 3: Findings & Recommendations Make recommendations that address the problems identified Recommendations may involve areas other then the coding department
The Audit Report Consider a standard format/house style for reports Will the same format be used for in-house reports? How will data be presented Consider confidentiality- use of a reference number instead of medical record number Use appendices for listing detailed information – e.g. details of all cases in the sample
The Audit Report Suggested Format Introduction Methodology Audit Findings e.g. Diagnoses Administrative DRG Conclusions Recommendations Appendices
The Audit Report Issue the report Keep a record of all audit documents and work to allow for queries by the hospital Enclose a covering letter arranging for follow up discussions Arrange any follow up promised by the report e.g. training
National Audit Maintain a library of audits Similar issues can arise in different hospitals Where inappropriate coding is identified – how will cases be rectified. Number of national audits Type of national audits Maintain audit skills – hospital and national
Computerised Audit Speeds up processes such as Identifying Population Creation of sample Data entry and re-grouping Collection of reasons for code differences Error categories Analysis of results Helps to maintain records of audits and outcomes to build a body of knowledge
Computerised Audit Consider Compatibility with hospital systems User friendly Creation of varied reports Ease of updating software if changes made to coding system Ownership of software Access to software
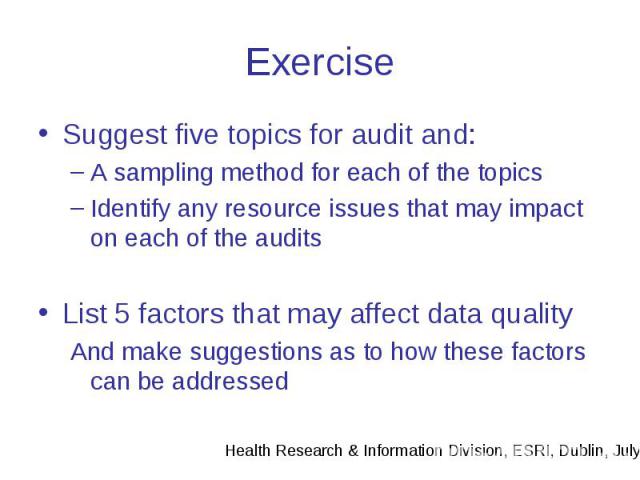
Exercise Suggest five topics for audit and: A sampling method for each of the topics Identify any resource issues that may impact on each of the audits List 5 factors that may affect data quality And make suggestions as to how these factors can be addressed